A1xLLcqAgt0qc2RyMz0y
Veteran
2019 Novel Coronavirus (SARS-CoV-2/COVID-19) for Dallas County Texas
https://www.dallascounty.org/departments/dchhs/2019-novel-coronavirus.php
https://www.dallascounty.org/Assets/uploads/docs/covid-19/press-releases/july/071620-PressRelease-DallasCountyReports1027AdditionalPositiveCOVID-19Cases.pdf
July 16, 2020 - 37,996 confirmed cases - 501 deaths
37,996 confirmed cases up 1,027 and sixteen new deaths
those 1,027 new cases represent a 2.8% increase over the last day
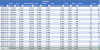
Increases (by percent) since March 27, 2020 :
21.0%, 19.6%, 11.1%, 12.5%, 14.9%
-- Month of April 2020 --
15.8%, 13.7%, 10.8%, 10.2%, 9.6%, 3.9%, 9.2%, 5.0%, 8.2%, 7.3%, 7.0%, 4.8%, 3.8%, 5.0%, 5.8%,
4.0%, 6.0%, 6.1%, 4.5%, 3.5%, 3.6%, 3.1%, 3.0%, 2.6%, 2.6%, 3.6%, 3.0%, 4.3%, 3.5%, 5.3%
-- Month of May 2020 --
5.3%, 4.9%, 6.0%, 5.7%, 5.9%, 5.3%, 5.2%, 4.9%, 4.7%, 4.5%, 4.3%, 3.9%, 3.8%, 3.6%, 2.9%, 3.0%,
2.8%, 3.0%, 2.9%, 2.4%, 2.3%, 2.5%, 2.0%, 2.1%, 1.9%, 2.1%, 2.1%, 2.2%, 2.1%, 2.2%, 2.3%
-- Month of June 2020 --
2.2%, 2.5%, 2.2%, 2.6%, 2.7%, 2.5%, 2.2%, 2.1%, 2.4%, 2.4%, 2.4%, 2.5%, 2.5%, 2.2%, 2.1%,
2.1%, 2.8%, 2.6%, 2.4%, 2.5%, 2.5%, 2.7%, 2.6%, 2.2%, 2.2%, 2.7%, 2.9%, 2.9%, 2.8%, 2.9%
-- Month of July 2020 --
2.5%, 3.2%, 4.8%, 4.7%, 4.3%, 4.7%, 4.0%, 3.7%, 4.1%, 3.8%, 3.5%, 3.6%, 3.3%, 2.9%, 2.9% and now 2.8%
Increases (by count) since March 27, 2020 :
+64, +72, +49, +61, +82
-- Month of April 2020 --
+100, +100, +90, +94, +97. +43, +106, +63, +108, +105, +107, +79, +65, +89, +109,
+80, +124, +134, +104, +84, +90, +81, +80, +71, +75, +105, +91, +135, +112, +179
-- Month of May 2020 --
+187, +181, +234, +237, +253, +246, +251, +249, +250, +251, +253, +236, +243, +235, +199, +214,
+205, +224, +225, +186, +183, +204, +172, +178, +171, +190, +197, +202, +200, +219, +228
-- Month of June 2020 --
+228, +257, +239, +285, +298, +289, +263, +254, +298, +300, +312, +328, +345, +302, +305,
+306, +413, +392, +394, +395, +408, +454, +445, +391, +403, +496, +561, +570, +572, +601
-- Month of July 2020 --
+544, +708, +1,085, +1,103, +1,062, +1,214, +1,077, +1,029, +1,201, +1,164, +1,101, +1,174, +1,114, +1,000, +1,055 and now +1,027
https://www.dallascounty.org/departments/dchhs/2019-novel-coronavirus.php
https://www.dallascounty.org/Assets/uploads/docs/covid-19/press-releases/july/071620-PressRelease-DallasCountyReports1027AdditionalPositiveCOVID-19Cases.pdf
July 16, 2020 - 37,996 confirmed cases - 501 deaths
37,996 confirmed cases up 1,027 and sixteen new deaths
those 1,027 new cases represent a 2.8% increase over the last day
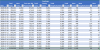
Increases (by percent) since March 27, 2020 :
21.0%, 19.6%, 11.1%, 12.5%, 14.9%
-- Month of April 2020 --
15.8%, 13.7%, 10.8%, 10.2%, 9.6%, 3.9%, 9.2%, 5.0%, 8.2%, 7.3%, 7.0%, 4.8%, 3.8%, 5.0%, 5.8%,
4.0%, 6.0%, 6.1%, 4.5%, 3.5%, 3.6%, 3.1%, 3.0%, 2.6%, 2.6%, 3.6%, 3.0%, 4.3%, 3.5%, 5.3%
-- Month of May 2020 --
5.3%, 4.9%, 6.0%, 5.7%, 5.9%, 5.3%, 5.2%, 4.9%, 4.7%, 4.5%, 4.3%, 3.9%, 3.8%, 3.6%, 2.9%, 3.0%,
2.8%, 3.0%, 2.9%, 2.4%, 2.3%, 2.5%, 2.0%, 2.1%, 1.9%, 2.1%, 2.1%, 2.2%, 2.1%, 2.2%, 2.3%
-- Month of June 2020 --
2.2%, 2.5%, 2.2%, 2.6%, 2.7%, 2.5%, 2.2%, 2.1%, 2.4%, 2.4%, 2.4%, 2.5%, 2.5%, 2.2%, 2.1%,
2.1%, 2.8%, 2.6%, 2.4%, 2.5%, 2.5%, 2.7%, 2.6%, 2.2%, 2.2%, 2.7%, 2.9%, 2.9%, 2.8%, 2.9%
-- Month of July 2020 --
2.5%, 3.2%, 4.8%, 4.7%, 4.3%, 4.7%, 4.0%, 3.7%, 4.1%, 3.8%, 3.5%, 3.6%, 3.3%, 2.9%, 2.9% and now 2.8%
Increases (by count) since March 27, 2020 :
+64, +72, +49, +61, +82
-- Month of April 2020 --
+100, +100, +90, +94, +97. +43, +106, +63, +108, +105, +107, +79, +65, +89, +109,
+80, +124, +134, +104, +84, +90, +81, +80, +71, +75, +105, +91, +135, +112, +179
-- Month of May 2020 --
+187, +181, +234, +237, +253, +246, +251, +249, +250, +251, +253, +236, +243, +235, +199, +214,
+205, +224, +225, +186, +183, +204, +172, +178, +171, +190, +197, +202, +200, +219, +228
-- Month of June 2020 --
+228, +257, +239, +285, +298, +289, +263, +254, +298, +300, +312, +328, +345, +302, +305,
+306, +413, +392, +394, +395, +408, +454, +445, +391, +403, +496, +561, +570, +572, +601
-- Month of July 2020 --
+544, +708, +1,085, +1,103, +1,062, +1,214, +1,077, +1,029, +1,201, +1,164, +1,101, +1,174, +1,114, +1,000, +1,055 and now +1,027
DALLAS -- As of 11:00am July 16, 2020, Dallas County Health and Human Services is reporting 1,027 additional positive cases of 2019 novel coronavirus (COVID-19), bringing the total case count in Dallas County to 37,996, including 501 deaths.
The additional 16 deaths being reported today include:
A man in his 30’s who was a resident of the City of Grand Prairie. He had been critically ill in an area hospital, and had underlying high risk health conditions.
A man in his 40’s who was a resident of the City of Mesquite. He expired in an area hospital ED, and did not have underlying high risk health conditions.
A man in his 40’s who was a resident of the City of Garland. He had been critically ill in an area hospital, and had underlying high risk health conditions.
A man in his 50’s who was a resident of the City of Irving. He had been critically ill in an area hospital, and had underlying high risk health conditions.
A man in his 60’s who was a resident of the City of Dallas. He had been critically ill in an area hospital, and had underlying high risk health conditions.
A man in his 60’s who was a resident of the City of Dallas. He had been critically ill in an area hospital, and did not have underlying high risk health conditions.
A man in his 60’s who was a resident of the City of Dallas. He had been critically ill in an area hospital, and had underlying high risk health conditions.
A man in his 60’s who was a resident of the City of Irving. He had been critically ill in an area hospital, and had underlying high risk health conditions.
A man in his 70’s who was a resident of the City of Dallas. He had been critically ill in an area hospital, and had underlying high risk health conditions.
A man in his 70’s who was a resident of the City of Lancaster. He had been critically ill in an area hospital, and had underlying high risk health conditions.
A woman in her 70’s who was a resident of the City of Grand Prairie. She had been critically ill in an area hospital, and had underlying high risk health conditions.
A man in his 70’s who was a resident of the City of Dallas. He had been hospitalized.
A man in his 70’s who was a resident of a long-term care facility in the City of Cedar Hill. He had been critically ill in an area hospital, and had underlying high risk health conditions.
A woman in her 80’s who was a resident of a long-term care facility in the City of Dallas. She expired in the facility, and had underlying high risk health conditions.
A woman in her 90’s who was a resident of a long-term care facility in the City of Dallas. She had been hospitalized, and had underlying high risk health conditions.
A woman in her 90’s who was a resident of the City of Dallas. She had been hospitalized, and had underlying high risk health conditions.
An increasing proportion of COVID-19 cases in Dallas County are being diagnosed in young adults between 18 to 39 years of age, such that of all cases reported after June 1st, half have been in this age group. Reports of cases are continuing to be associated with multiple large recreational and social gatherings since the beginning of June. Of the cases requiring hospitalization to date, more than two-thirds have been under 65 years of age. Diabetes has been an underlying high-risk health condition reported in about a third of all hospitalized patients with COVID-19.
The percentage of respiratory specimens testing positive for SARS-CoV-2 was 30% among symptomatic patients presenting to area hospitals in week 27. Of cases requiring hospitalization who reported employment, over 80% have been critical infrastructure workers, with a broad range of affected occupational sectors, including: healthcare, transportation, food and agriculture, public works, finance, communications, clergy, first responders and other essential functions.
Of the 501 total deaths reported to date, about a third have been associated with long-term care facilities.